Understanding the ever changing influenza virus can be an arduous undertaking, to say the least. However, this task can become more manageable by examining the most common and two main types, including Types A and B. These types are routinely spread in humans and give rise to the infamous and unwavering seasonal flu epidemics each year. The influenza virus is made more complicated because type A can further be broken down into sub-types depending on the expressed surface proteins. In fact, in any given season, a variety of versions of types (A & B) and subtypes (influenza A) can circulate and infect individuals leading to its infectious disease.
Influenza infections are caused by a virus that acts on an individual’s respiratory system. Common port of entry include the nose, eyes and mouth. The flu viruses can survive in the air in droplets when an infected person coughs, sneezes or even talks, that can later be transmitted directly by inhalation, or indirectly from touching germ-laden fomites. The most susceptible patients are young children (especially under 12 months), the elderly (65+ years), and others with compromised immune systems. Symptoms may start off feeling like a common cold, with indications encompassing a runny nose, sneezing and sore throat. Nevertheless, a key distinction is that influenza is an acute infection and symptoms tends to come on suddenly and the infectious process usually leaves patient’s feeling much worse with the flu. Additionally, the flu can progress to worsening conditions such as asthma flare-ups, bronchitis, pneumonia and even death.
To elaborate on the severity of the influenza epidemic, so far for the 2019-2020 season (October 1, 2019- February 1, 2020), there’s been an estimated 22-31 million cases of flu illness, 210-370 thousand flu-related hospitalizations and 12-30 thousands deaths caused by flu. Consequently, the risk of coming down with the the flu or suffering the consequence of death is significantly reduced by getting an influenza vaccine each year. The flu shot provides around 50-60% protection for those 16-64 years of age. This is mostly due to the rapid and ever evolving virus due it’s capacity for antigenic drift. Therefore, each year, scientist only can provide a “guess-timation” of 3-4 potential virus for a given year. Additionally, an annual shot is needed because immunity decreases with time. In short, some protection is better than none.
For the 2019-2020, the flu vaccine has the following components depending on whether you receive the Trivalent or Quadrivalent vaccine.
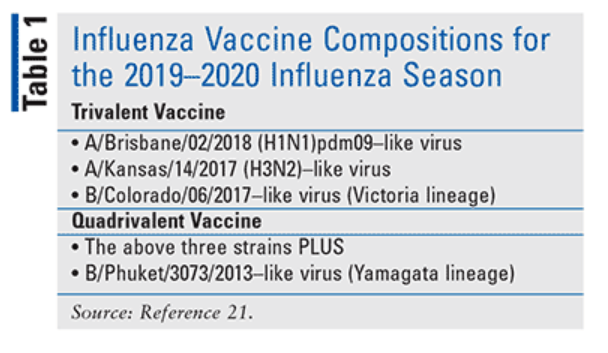
So far, it is estimated to have 40-60% effectiveness. In addition to flu vaccine which can protect you against 3 or 4 viruses that research suggests will be most common, there are other ways to prevent from getting the flu. This includes 5 simple tips.
- Avoiding close contact with those known to have the flu,
- If you are sick with the flu, do not attend school or work to avoid spreading the flu
- Cover your mouth and nose with tissue when you cough or sneeze or sneeze into your elbow
- Avoid touching your face. Particularly, the virus spreads by touching your eyes, nose and mouth
- Wash your hands frequently with soap and water